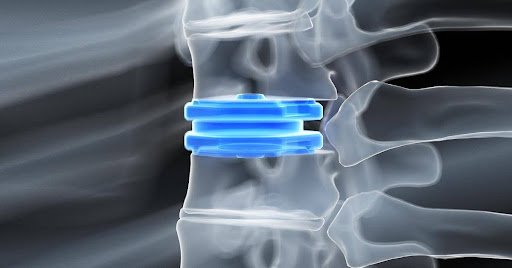
Spinal disc replacement has emerged as a life-changing option for patients with chronic back or neck pain caused by degenerative disc disease. While surgical techniques and implant materials have significantly evolved, the methods used to assess recovery and long-term success continue to advance as well. Among these, advanced motion analysis technology is transforming how clinicians evaluate spinal disc replacement outcomes. Dr. Larry Davidson, a recognized leader in minimally invasive spinal surgery, highlights that incorporating motion analysis into post-surgical care allows for a deeper, more precise understanding of functional recovery. With greater insight into patient movement and biomechanics, this technology is reshaping post-operative care and optimizing patient outcomes.
What Is Motion Analysis Technology?
Motion analysis technology refers to a suite of tools and systems that objectively measure how the body moves. It typically includes high-speed cameras, reflective markers, pressure sensors and force plates, all of which work together to generate a 3D representation of body motion. In spinal surgery, these systems can be used to analyze the mobility of specific spinal segments, detect compensatory movements and quantify the range of motion restored by artificial disc implants.
Unlike subjective observations or patient-reported outcomes, motion analysis offers quantifiable data. Clinicians can use these metrics to assess whether a spinal disc replacement has achieved its goal of preserving or improving motion while alleviating pain. This level of precision supports more tailored rehabilitation plans and enables earlier intervention if the recovery process veers off track.
Evaluating Biomechanical Function Post-Surgery
A major goal of spinal disc replacement is to restore natural spinal movement. Advanced motion analysis allows clinicians to measure this recovery with great accuracy. By examining spine mechanics during activities such as walking, bending and twisting, practitioners can determine how well the artificial disc is functioning in comparison to a healthy spinal segment.
Motion analysis systems collect data on joint angles, segmental mobility and posture alignment. These parameters are particularly important in identifying whether a patient is compensating with other body parts due to limited spinal movement. If such patterns are detected, targeted physical therapy can be implemented to correct them, ensuring a more balanced and sustainable recovery.
Personalized Rehabilitation Through Data-Driven Insights
One of the most significant advantages of motion analysis technology is its ability to guide personalized rehabilitation programs. Each patient’s recovery journey is unique and real-time movement data enables therapists to adjust treatment plans accordingly. For example, if motion analysis reveals restricted rotation or asymmetry in gait, specific exercises can be introduced to target those deficiencies.
This tailored approach results in more efficient rehabilitation, as therapy focuses on precise functional limitations rather than general mobility improvement. Patients benefit from faster recovery times, fewer complications and a higher likelihood of regaining full function.
Monitoring Progress Over Time
Another key benefit of motion analysis is its ability to track progress over time. Periodic assessments throughout the post-operative period provide clinicians with a clear picture of how the patient’s movement evolves. Any plateau in recovery or regression in mobility can be quickly identified and addressed.
This longitudinal data is especially useful in evaluating the long-term performance of different types of spinal disc implants. By comparing movement patterns at various stages immediately after surgery, at three months, six months and one year, clinicians can assess the durability and functional longevity of the implant.
Comparing Pre- and Post-Surgical Mobility
One of the most compelling uses of motion analysis is the comparison between pre- and post-surgical mobility. By capturing motion data before the procedure and continuing after recovery begins, clinicians can directly measure improvement or identify new movement challenges that may arise postoperatively.
These comparisons help set realistic expectations and can be shared with patients to demonstrate tangible progress. They also serve as an educational tool, helping patients better understand the role of proper biomechanics in recovery and daily movement.
Applications Beyond the Clinic
With the rise of wearable motion sensors and mobile platforms, motion analysis technology is expanding beyond the confines of specialized labs. Patients can now wear compact devices that monitor their movements during daily activities at home. This remote monitoring approach provides clinicians with a more holistic view of recovery in real-world conditions.
Data collected from wearable devices can be uploaded to cloud-based systems, where AI algorithms analyze trends and detect anomalies. If abnormal patterns emerge, such as reduced range of motion or excessive strain on a specific area, clinicians are alerted to intervene early. This not only enhances patient safety but also contributes to more dynamic and adaptive care.
Enhancing Surgical Techniques and Implant Design
Beyond immediate patient care, motion analysis also helps refine surgical techniques and improve implant design. By analyzing how different implant models influence spinal biomechanics, researchers and manufacturers can make evidence-based modifications that improve performance.
Surgeons can also use motion analysis data to evaluate their surgical outcomes more critically. If consistent movement restrictions or complications are observed across multiple patients, technique adjustments can be explored to improve future results. In this way, motion analysis contributes to both individual patient outcomes and broader advances in spinal surgery.
Challenges and Considerations
While the benefits of motion analysis are clear, there are practical considerations for implementation. The technology can be costly and specialized training is often required to operate the equipment and interpret the data accurately. Additionally, access to motion analysis labs may be limited in rural or under-resourced healthcare settings.
To overcome these barriers, healthcare providers are increasingly adopting more affordable and accessible mobile and wearable solutions. Collaboration between hospitals, outpatient clinics and rehabilitation centers can also expand the availability of motion analysis services to a wider patient population.
Advanced motion analysis technology is revolutionizing the way spinal disc replacement outcomes are measured and understood. By providing objective, data-driven insights into functional recovery, this technology enables more personalized care, quicker interventions and improved long-term outcomes.
Dr. Larry Davidson emphasizes, “Minimally invasive spinal surgical techniques have resulted in a decrease in the length of certain surgeries, hospitalization time, potential for postoperative infection, and readmissions to the hospital.” These improvements align closely with the objectives of motion analysis technology, which seeks to complement surgical advances by enhancing recovery monitoring and long-term patient support. As this technology continues to evolve and become more accessible, it holds the promise of raising the standard of care for spinal disc replacement patients across the globe.